Age-related macular degeneration
Age-related macular degeneration is the main cause of severe visual disability among the elderly. The onset of the disease is often insidious, gradual and painless but sometimes results in a sudden severe loss of eyesight.
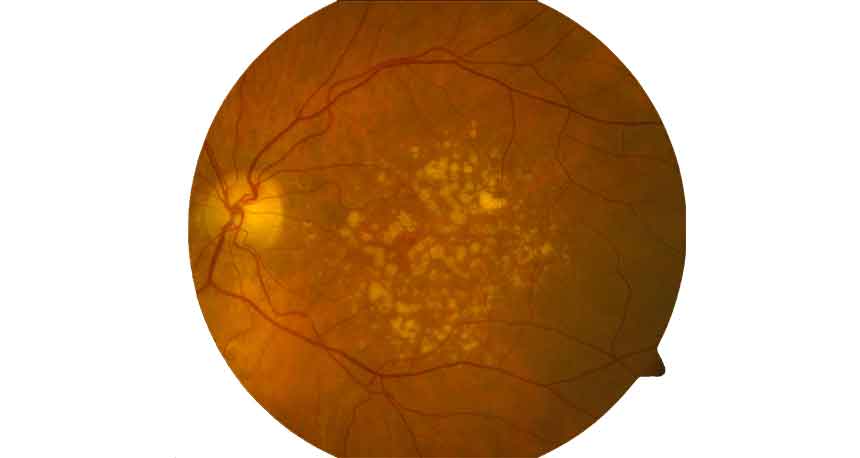
Age-related macular degeneration begins with characteristic yellow deposits (drusen) at the pigment epithelial layer of the retina. During the visual process, the photoreceptors of the retina produce different metabolic products that are normally removed. In the case of macular degeneration, however, these substances remain, as if the cells‘ waste disposal system had stopped working properly.
In the “dry” form of AMD, the deposits gradually disappear, but the photoreceptors above the deposits disappear with them, leaving an atrophic scar (see photo). Most AMD patients (approx. 80%) suffer from this common form.
In 20% of the cases, inflammation occurs as a reaction to formation of the deposits. This inflammatory reaction may lead to abnormal blood vessel growth, which progressively spreads beneath the retina. Such abnormal growth leads to bleeding, leaking and scarring, and may leave behind massive scar tissue in the advanced phases if left untreated. Such changes lead to sudden, abrupt deterioration of eyesight, especially when reading. Patients generally notice this when spots appear or words and lines are perceived as distorted or bent. In some cases, facial recognition may become difficult. In any case, a sudden deterioration of eyesight generally occurs.
The most important factors influencing AMD are age and genetic predisposition. Smoking, high blood pressure and poor diet may also help trigger the illness, however.
Wet AMD

Dry AMD
The current treatment options are
- Intravitreal injection (IVI) of anti-angiogenic drugs: these drugs are injected directly into the vitreous humour of the eye. The substances in these drugs specifically inhibit abnormal blood vessels, especially targeting the molecules that exacerbate their growth. This therapy promises improved vision in approx. 30%-40% of all patients. IVI is administered in the form of outpatient therapy, and is performed in the practice. A variety of drugs are available, depending on the patient’s disease.
- Photodynamic therapy: In this treatment, the patient receives an infusion with a specific, photosensitive drug. The eye is then irradiated with a weak laser beam, which activates the drug that subsequently inhibits blood vessel growth. This therapy is usually used in combination with IVI, because when it is used alone it merely stabilises the condition rather than leading to an improvement.
- Laser: In certain, rare, cases, lasers may be used to destroy or seal off new blood vessels. Laser therapy leads to the irreversible formation of blind spots, however, so it is used only in very few, select cases.
- Combined therapies: Generally, the above-mentioned therapies may be combined for greater effect.
- Photobiomodulation: Photobiomodulation is a treatment modality for certain forms of intermediate and/or dry age-related macular degeneration (AMD). Using different wavelengths of visible light which irradiate the macula, specific cellular components in the lowest layer of the retina (so-called mitochondria) are activated and lead to the removal of deposits (so-called drusen) which have accumulated in the macula. The treatment is generally very safe and has very few side-effects. There are some studies which underline its efficacy, but the data are not as robust as those for treatments of wet or neovascular AMD. As it is a very mild treatment, it can, however, be an interesting alternative for certain patients.

